Unique Psychiatry Program Delivers De-Stigmatized, Compassionate Care
It’s a sobering fact that people with severe mental illness than the rest of the population. But the cause isn’t what you might expect, according to Marsha Wittink, MD, chief of academic affairs in the division of Medicine in Psychiatry Services (MIPS) at the University of Rochester Medical Center.
“The reason these patients die early is multi-factorial, but it’s important to realize they are dying from common chronic medical conditions such as diabetes, heart disease, COPD and cancer—the same basic medical conditions we are trying to prevent in the general population.”
Wittink, who is trained in family medicine and studies the integration of mental and physical health, is one of a growing number of clinicians trying to help this patient population that struggles with access to quality medical care.
For those dealing with bipolar disorder or schizophrenia, tasks like making appointments or following up on instructions can quickly become overwhelming, in part because they are more likely to face social barriers such as housing and food insecurity, but also because .
As a result, many fail to go to primary care visits where health issues can be prevented or detected and treated early. These health barriers only grow worse when patients have acute medical illnesses and need to be admitted to the hospital.
Wittink, who calls the situation “deplorable,” has worked with colleagues to when it comes to decreasing length of stay and readmissions, and helping patients remain in the community.
Whether it’s a quick visit or longer hospital stay, past experiences have made many of these patients feel misunderstood or unsafe in health care settings. So, what can medical providers do to make these patients feel comfortable, safe, and taken seriously when they need help?
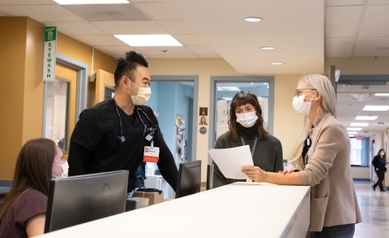
The MIPS approach to that question can be summarized in three words: compassion, collaboration, and creativity.
Meeting People Where They Are

URMC’s structure, which combines three services that work together, makes it one of the most innovative programs in the country. Today, the MIPS Primary Care (MIPS-PC) office is a full-service physician practice next to Strong Ties on the URMC Brighton Campus on West Henrietta Road. They take outside referrals in addition to seeing many patients already receiving care at Strong Ties and Strong Recovery.
In 2007, MIPS added an inpatient unit at Strong Memorial on 1-9200 (IMIP) with 10 medical beds, that soon grew to 20 beds in 2010, for severely mentally ill patients admitted for acute medical concerns such as exacerbation of congestive heart failure, acute kidney injury, or pneumonia. Finally, in 2021, MIPS added a third service: a 10-bed unit on G-9200 (SUMMITS) for patients with acute medical needs and substance use disorders.
The unique structure of MIPS helps minimize obstacles their patients face, since those with severe mental illness carry a lot of baggage when it comes to medical care. At MIPS-PC, patients may be wary of blood draws, concerned about removing clothing or being touched during medical exams. These concerns are honored in a way that’s tailored for each patient.
Giving patients dignity and some control is one simple way MIPS seeks to build a foundation of trust, explains Kevin Brazill, DO, a dual-boarded family medicine physician and psychiatrist who is the medical director of the MIPS primary care clinic.
“It’s a cliché, but the main thing is meeting people where they are and allowing them to help create an agenda for their first meeting,” he said. “It’s rare for patients to be asked what they want when they come to the doctor. We explain that if they need to be in the hospital, we have a special unit where we work with partnering docs and nurses to make sure they know their care is streamlined.”
Wittink is the medical director of the IMIP unit and Kirk Harris, MD, dual-boarded internist and psychiatrist, is the medical director of the SUMMITS unit. Many clinicians involved with the program float between one or more of the services.
Teams from each area, including nurses, physicians, social workers, care-coordinators, psychologists, pharmacists, and more recently peer-advocates, from each area meet regularly to talk about patients, many of whom overlap, depending on their needs. MIPS also holds weekly lectures and case presentations for its clinical staff, students and residents to discuss research related to combined medical and psychiatry care and team-based interventions.
While collaboration is the driving force within the MIPS care team, part of the challenge lies in making others aware of the program’s role within the Medical Center.
The MIPS division has a strong history of continuous quality improvement led by nurse leaders such as Lorraine Schild, NP, Robert Balme, RN, Stephanie McClure, RN and Jennifer Hart, RN. Recently the team received a Quality Institute grant to support the creation and implementation of a that prompts patients to answer a series of questions on an iPad.
When the tool was piloted with patients on 1-9200, patients were asked to rank their priorities in order of importance. Early data showed that most ranked “Managing my emotions” and “Understanding my health” as their top priorities. That summarizes the whole point of Med-Psych, Wittink said.
“This is a model that is critical for this population, but quite frankly, I would want this for my own family. It’s a comprehensive way to deliver medicine the way all of our patients deserve.”
How MIPS Started
Telva Olivares, MD, co-founder of the MIPS division and its outgoing clinical chief, has dedicated her career to going the extra mile, literally in some cases. Jennifer Hart, RN, assistant nurse manager at MIPS, remembers going with Olivares into a clinic parking lot to do a blood draw on a patient who was hesitant to step inside. “We work together to make sure our patients are cared for, no matter where we have to meet them,” Hart said.
Olivares saw early on how these patients can fall through the cracks. As a dual psychiatry and internal medicine resident at the University of Rochester, she remembers meeting a woman with a psychiatric disorder whose breast cancer had metastasized completely.
“Everybody thought she was delusional or pregnant with heavy back pain,” said Olivares, who recalls similar scenarios: Patients with broken bones that never healed properly because they never got care or cut off their cast too soon. Or those with uncontrolled diabetes or high blood pressure. “I kept thinking about the opportunities that could arise from giving people that had severe mental illness prompt care,” she said.
Olivares became one of the first people to train in URMC’s first dual Medicine and Psychiatry residency in the 1990s—which was an innovative program that combined medicine and psychiatry (this training program was eventually discontinued in 2002, but she and others would like to change that).
She crossed paths with faculty including Roger Boulay, MD, and then-Chair of Psychiatry Eric Caine, MD, who would become valuable mentors for her as well as champions of this two-tiered approach to preventive care.
Soon, an opportunity appeared in plain sight. The Strong Ties facility served as a hub for outpatient psychiatric care, day treatment programs, and (eventually) a pharmacy. Patients often stuck around to have lunch or socialize in the parking lot over cigarettes. It was the perfect place to start.
It was 1995 when Boulay and Olivares, who was a third-year resident at the time, set up a makeshift clinic in the Strong Ties parking lot. They started by giving free flu shots to Strong Ties patients. The same people started coming back with medical needs and as the need grew, the doctors moved into a room inside the clinic.
That room turned into a formal outpatient clinic for patients with psychiatric needs as the team began adding staff and space. By the time Boulay retired and Olivares became an attending physician in 1999, MIPS was set up for further growth.
It hasn’t stopped growing since, and Olivares says the reason is simple: “It’s not just about medical needs,” she said. “We look at the welfare of our patients. We know our role is unique in that we’re probably the only human contact they have that day, so we want to make it meaningful.”
Learn more
Visit the Medicine in Psychiatry Services (MIPS) website.


